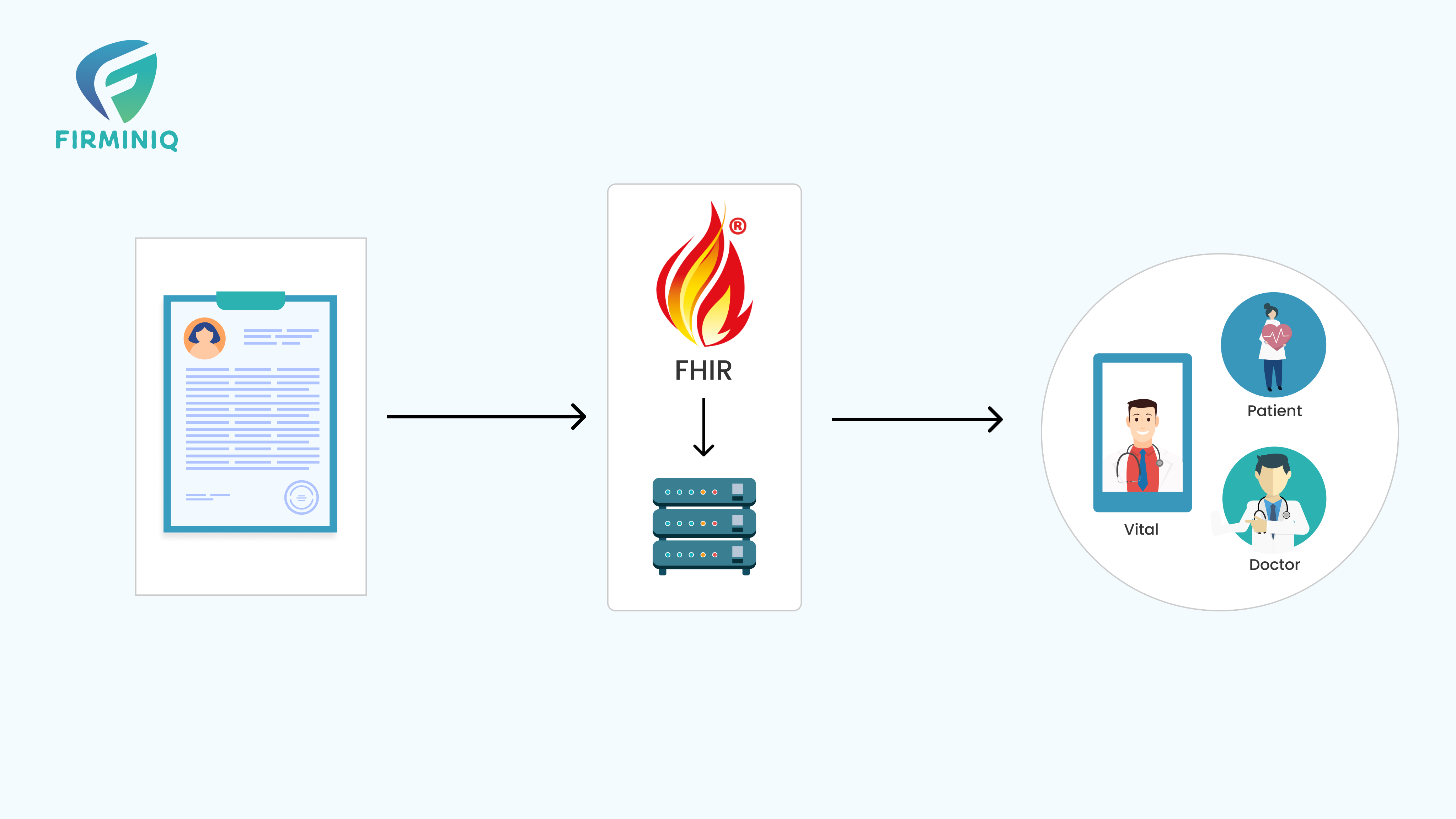
What is HL7 FHIR?
The Fast Healthcare Interoperability Resources (FHIR) represents the next phase in interoperability standards within the healthcare sector, developed by the standards development organization, HL7. This framework serves as a pivotal standard for the electronic exchange of healthcare information. It emphasizes the crucial prerequisites of data accessibility, discoverability, and comprehensibility. FHIR advocates for structured and standardized data formats to bolster clinical decision-making processes and facilitate machine-based data handling for healthcare processed.
What is HL7?
Health Level 7 (HL7) has been actively engaged in resolving the hurdles associated with healthcare data exchange since its inception in 1987. Over the years, it has pioneered information modeling standards such as HL7 V2 and HL7 V3. As the healthcare domain witnesses an influx of new data, HL7 remains committed to evolving its standards. Notably, the HL7 FHIR emerges as the latest specification in their repertoire, reflecting the organization’s ongoing efforts to adapt to the changing landscape of healthcare data exchange.
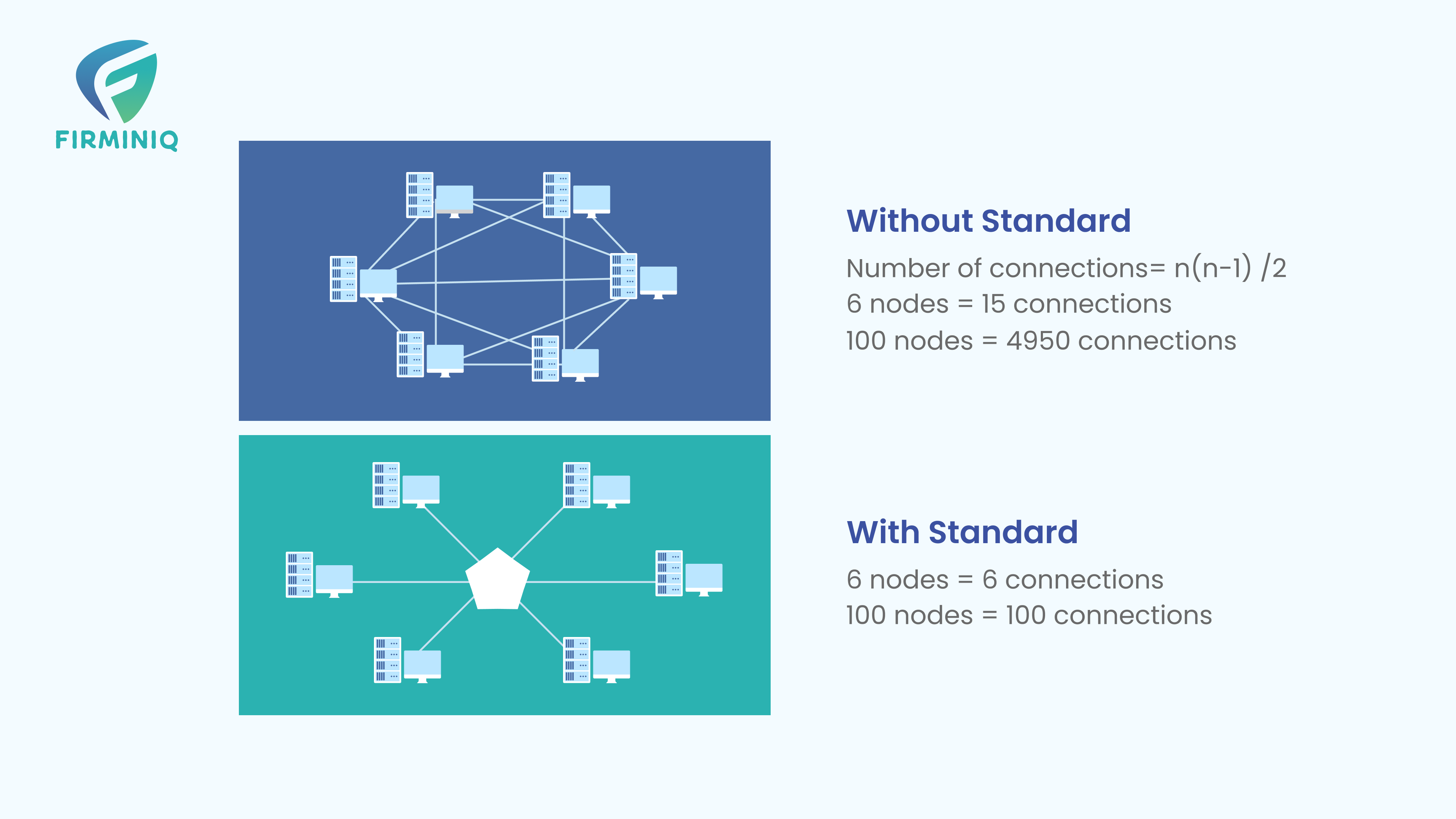
The Need for Standards
To illustrate with the below figure, without any standard, between 6 nodes we would require approx. 5000 connections. Imagine, if the number of nodes reaches 1 million. With some standards in picture, the number of connections gets limited to the number of nodes in the system.
Why do we need FHIR?
- Simplifies implementation while upholding information integrity as a primary objective.
- FHIR leverages established patterns and content models as its foundational building blocks.
- Offers flexibility as it can function autonomously for data exchange or complement existing widely adopted standards.
- Employs RESTful FHIR APIs for streamlined and efficient data exchange methodologies.
- Represents healthcare data through evolving vocabularies, terminologies, and codes, adapting to dynamic changes over time.
- Customizable to align with specific requirements and needs.
Components of FHIR
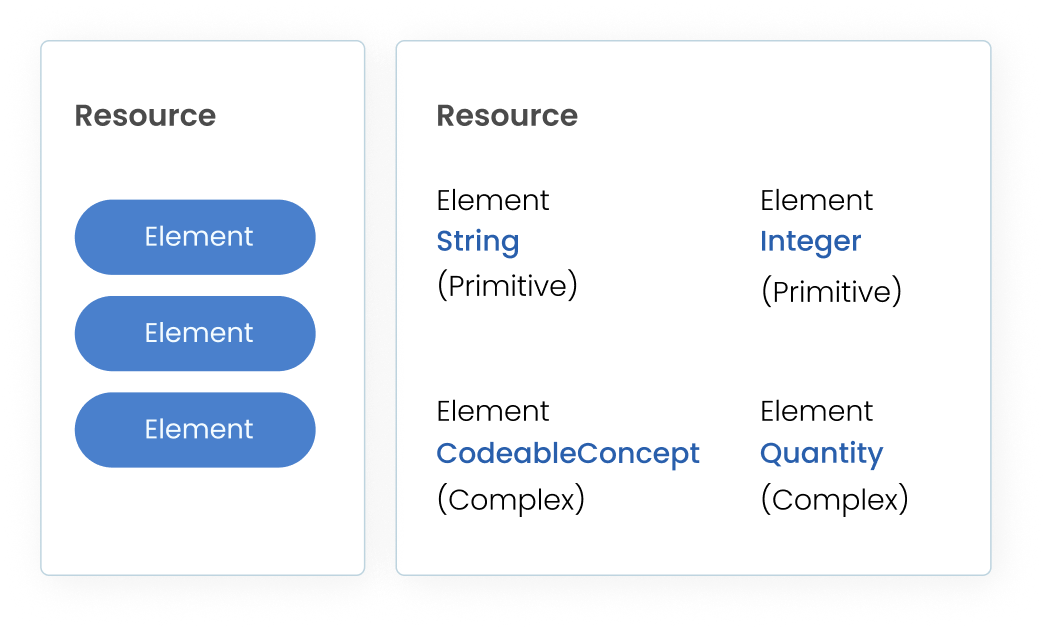
1. Resources
FHIR delineates all shareable content as resources, encompassing entities such as Patient, Practitioner, Person, Encounter, Observation, Diagnosis, and more. With approximately 150 resources, FHIR embodies diverse healthcare domains through each distinct resource. Each of these resources comprises specific elements integral to its structure.
2. Elements
An element represents the most granular unit of data within the system. Every element is associated with a designated data type that defines its specific nature. These types categorize into either Primitive or Complex classifications.
Primitive types consist of single values, while Complex types amalgamate multiple primitive data types. Complex data types have the capacity to include nested structures of additional complex data types.
3. Terminology Binding
Certain elements within FHIR necessitate the selection of a value from a specific terminology. For instance, the administrative gender of a patient allows for values like male, female, other, or unknown.
Terminology binding in FHIR refers to the specification requiring certain elements to align with predefined terminologies or vocabularies for accurate and consistent data representation. This ensures that specific data elements correspond to designated terminologies, enhancing interoperability and comprehension across healthcare systems. Flexibility exists within the system to configure elements to align with preferred terminologies.
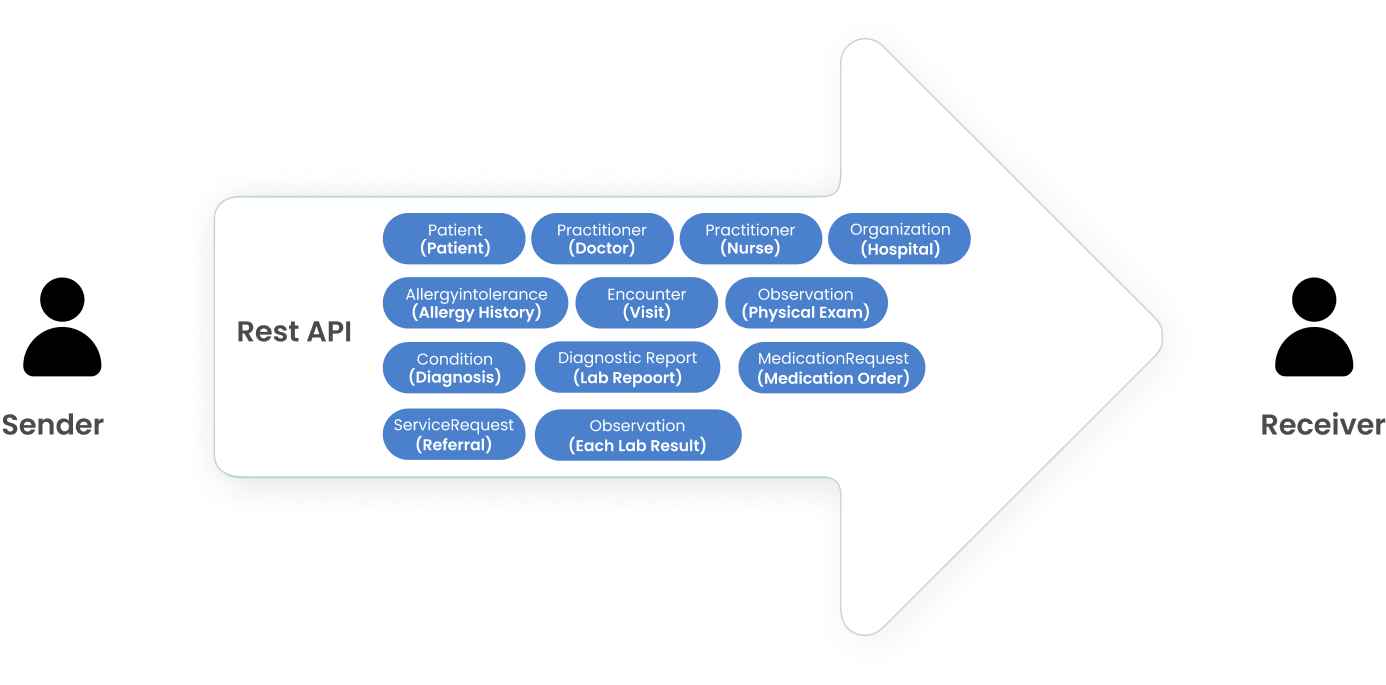
4. Exchange Mechanism
Once we organize our data into resource formats, the subsequent step involves transmitting these resources to other entities through the REST API. This process commonly involves the transfer of multiple resources in a single interaction, streamlining the exchange of information between systems or users.
The exchange mechanism in FHIR describes the methodology employed for sharing healthcare information between different systems or entities. It outlines the standardized approach and protocols utilized to facilitate seamless data exchange, promoting interoperability and communication within the healthcare ecosystem.
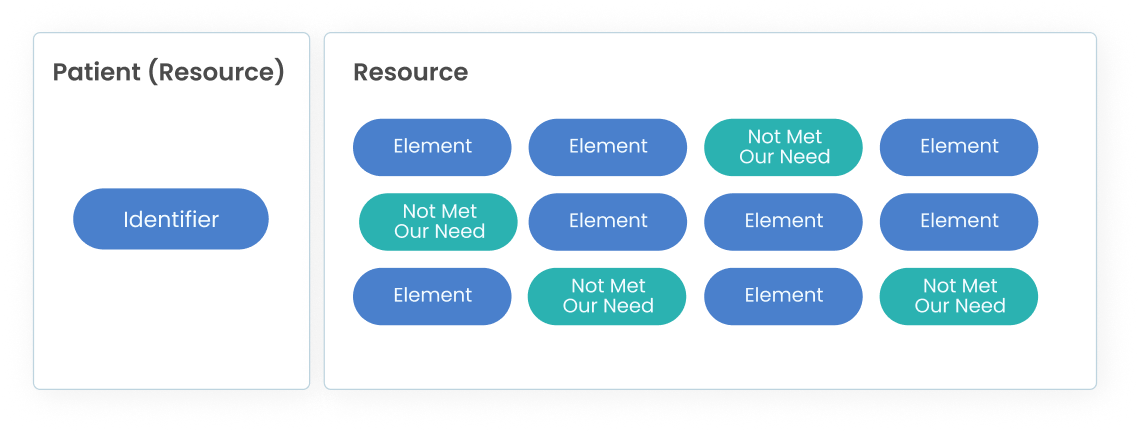
5. FHIR Profiling
FHIR resources are designed for general purpose use, but we can customize it to meet our context.
6. Implementation Guide
Within a specific exchange scenario, numerous profiles, extensions, terminology bindings, and associated guidelines are crafted. These elements, when consolidated into a cohesive set of FHIR resources tailored for a particular exchange context, collectively form what is termed an Implementation Guide (IG). Notable examples of IGs include the US Core Implementation Guide, focusing on exchanging comprehensive patient data within the US, and the International Patient Summary (IPS) Implementation Guide, facilitating the exchange of patient summaries across different countries.
FHIR Pros
1. Interoperability
FHIR enables seamless data exchange between different healthcare systems, fostering interoperability. Its standardized format ensures information can be shared efficiently across various platforms and devices.
2. Scalability and Flexibility
It supports a wide range of data types and is adaptable to evolving healthcare needs. FHIR’s modular approach allows for easy integration with existing systems, promoting scalability without major disruptions.
3. Improved Patient Care
By facilitating access to comprehensive and up-to-date patient data, FHIR assists healthcare providers in making informed decisions, leading to improved diagnosis and treatment.
4. Enhanced Efficiency
FHIR streamlines workflows by enabling quicker access to relevant patient information. This reduces administrative burdens, minimizes errors, and optimizes resource utilization.
5. Patient Empowerment
FHIR promotes patient engagement by granting individuals better access to their health records. This fosters a more active role in their own care and facilitates communication with healthcare providers.
6. Innovation and Integration
Its modern, web-based approach encourages innovation in healthcare technologies. FHIR’s compatibility with emerging tech, like IoT devices and mobile apps, supports their seamless integration into healthcare ecosystems.
7. Compliance and Security
FHIR adheres to stringent security standards, ensuring data privacy and compliance with regulations like HIPAA. Its granular data access controls enhance security measures.
8. Cost-Efficiency
Implementing FHIR can lead to cost savings by reducing redundancies, streamlining processes, and minimizing the need for custom interfaces.
9. Research and Analytics
FHIR’s standardized data format facilitates research and analytics initiatives. It enables the aggregation of data from diverse sources for comprehensive analysis, leading to insights that can drive advancements in healthcare.
FHIR Cons
1. Complex Implementation
Integrating FHIR into existing systems can be intricate and time-consuming. Legacy systems might require substantial modifications to align with FHIR standards, posing challenges during the transition phase.
2. Costs and Resource Allocation
The initial investment for FHIR integration, including software upgrades, staff training, and system customization, can be significant. Additionally, ongoing maintenance and updates may strain financial resources.
3. Interoperability Challenges
While FHIR promotes interoperability, achieving seamless data exchange among disparate systems, especially those using different versions of FHIR or other standards, can be complex. Inconsistencies in data formatting or interpretation may arise.
4. Data Governance and Standardization
Maintaining data consistency and ensuring adherence to FHIR’s standards across various platforms and organizations could pose governance challenges. Differing interpretations of FHIR’s guidelines might lead to data discrepancies.
5. Security Risks
Despite robust security measures, integrating multiple systems through FHIR can potentially create new vulnerabilities or increase the attack surface, requiring stringent security protocols and continuous monitoring.
6. User Adoption and Training
Healthcare professionals might face a learning curve when transitioning to FHIR-based systems, impacting productivity during the initial phases. Adequate training and change management strategies become imperative.
7. Vendor Support and Compatibility
Ensuring that all vendors and systems involved in data exchange are FHIR-compliant might pose challenges. Incompatibility issues between systems from different vendors could hinder seamless interoperability.
8. Regulatory Compliance
Compliance with evolving healthcare regulations and standards while incorporating FHIR might demand ongoing adjustments and updates, adding complexity and potential compliance risks.
HTTP Interactions with FHIR Resources
Following are the most commonly used HTTP Interactions:
- Read: Retrieves a specific resource by its unique identifier
- Vread: Fetches a specific version of a resource by its version identifier
- Update: Modifies or replaces a specific resource identified by its unique identifier.
- Patch: Applies partial modifications to a specific resource.
- Delete: Removes a particular resource based on its identifier.
- Create: Generates a new resource within the specified resource type.
- Search: Retrieves resources matching specified search parameters within a resource type.
FHIR Servers
FHIR servers, based on the Fast Healthcare Interoperability Resources (FHIR) standard, serve as crucial components in healthcare data management by facilitating the exchange and access of electronic health information.
A server that utilizes FHIR APIs and FHIR Resources for data exchange can fall into two categories:
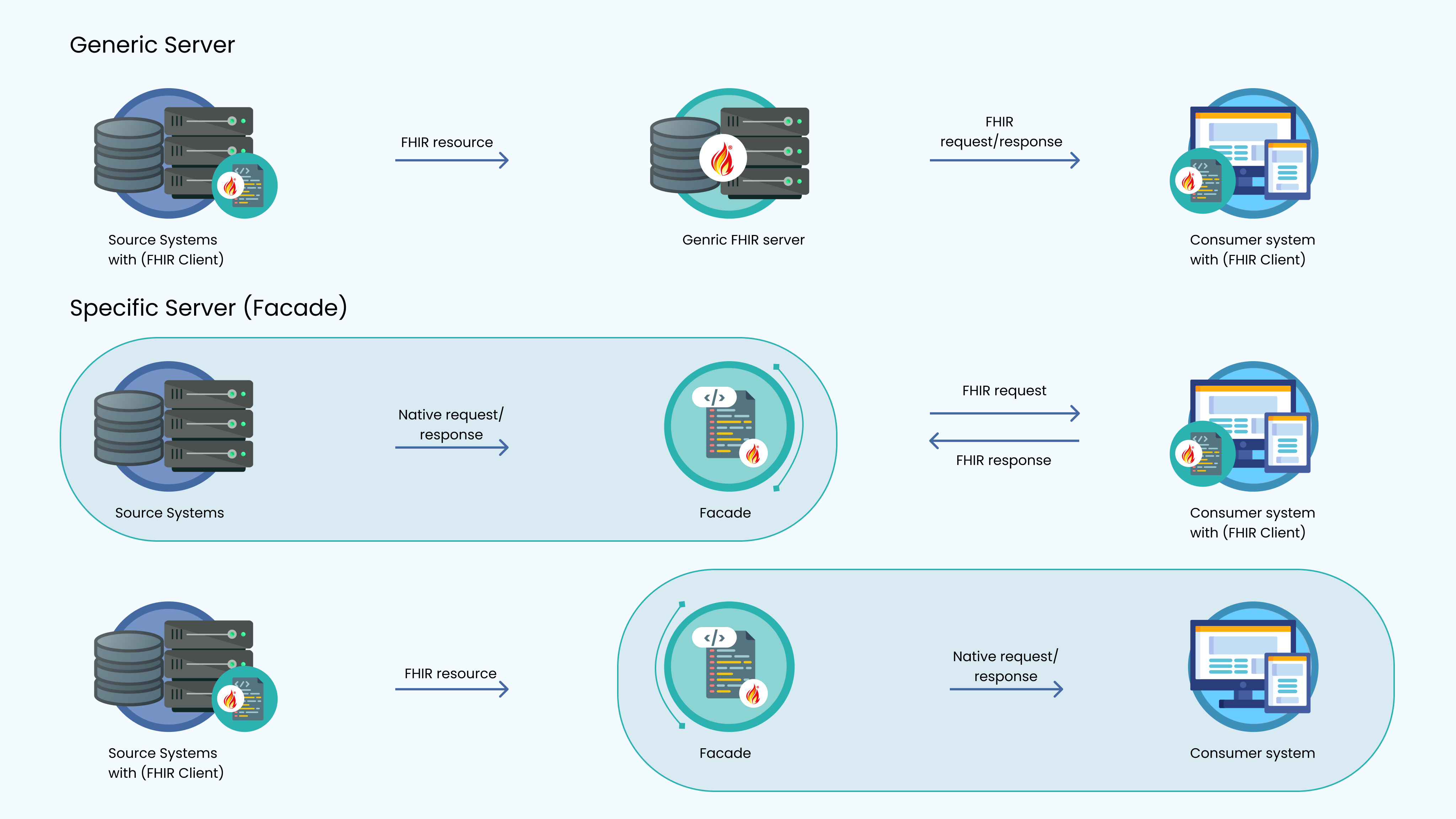
Generic Server
This type fully supports all interactions and standard resources within FHIR, incorporating its own data storage capabilities.
Specific Server (Facade)
This server selectively implements a portion of the API tailored for specific use-cases, lacking independent data storage functionalities.
Open source FHIR servers available in the market
Below are the commonly used FHIR Servers available in the market
- HAPI FHIR
- Firely Team/Spark
- Asymmetric FHIR API Server
- IBM FHIR Server
- FHIR Server for Azure
- FHIR Works on AWS
Commercial FHIR servers available in the market
Some common commercial FHIR servers are listed below
- SMILE CDR
- Azure API for FHIR
- Firely Server
- Google Cloud HealthCare
- Aidbox
- Helios
Conclusion
In conclusion, adopting FHIR for healthcare interoperability offers a transformative approach, enabling seamless data exchange and enhancing collaboration across diverse systems. The utilization of FHIR’s standardized resources and protocols not only streamlines information sharing but also facilitates comprehensive and secure data handling. Embracing FHIR empowers healthcare entities to achieve greater efficiency, interoperability, and adaptability within their ecosystems, ultimately fostering improved patient care, streamlined workflows, and enhanced decision-making processes.