In many parts of the world, delivering consistent, high-quality care remains a daily challenge, especially in rural and low-resource settings. Limited infrastructure, stretched workforce, and widespread chronic illness often hinder timely care. But technology is changing the narrative. Remote Patient Monitoring (RPM) is not just a buzzword; it’s a lifeline that’s redefining how care is accessed and delivered in underserved regions.
By embracing RPM, healthcare providers can extend their reach beyond clinic walls, empower patients with proactive care, and make data-driven decisions, all without massive infrastructure or budget overhauls. The key lies in choosing the right tools & partners, training the right people, and building workflows that fit the context.
In this post, we explore step-by-step strategies to implement RPM effectively in low-resource environments—so one can deliver impactful, scalable, and sustainable care where it’s needed the most.
Understanding the Challenges of Low-Resource Settings
Before diving into the implementation, it’s essential to recognize the challenges healthcare providers face in low-resource environments:
- Limited infrastructure: Poor internet connectivity, lack of electricity, and inadequate healthcare facilities hinder smooth adoption of technology.
- Healthcare workforce shortages: Rural areas often struggle with limited access to trained doctors, nurses, and technicians.
- Patient awareness and literacy: Many patients may be unfamiliar with digital tools, making onboarding a challenge.
- Budget constraints: Financial limitations prevent investment in sophisticated technology and high-end devices.
Effective RPM deployment in rural and regional areas is viewed by health professionals as crucial for bridging healthcare divides. – BMC Health Services Research
Why RPM is a Game Changer in Rural and Low-Resource Areas
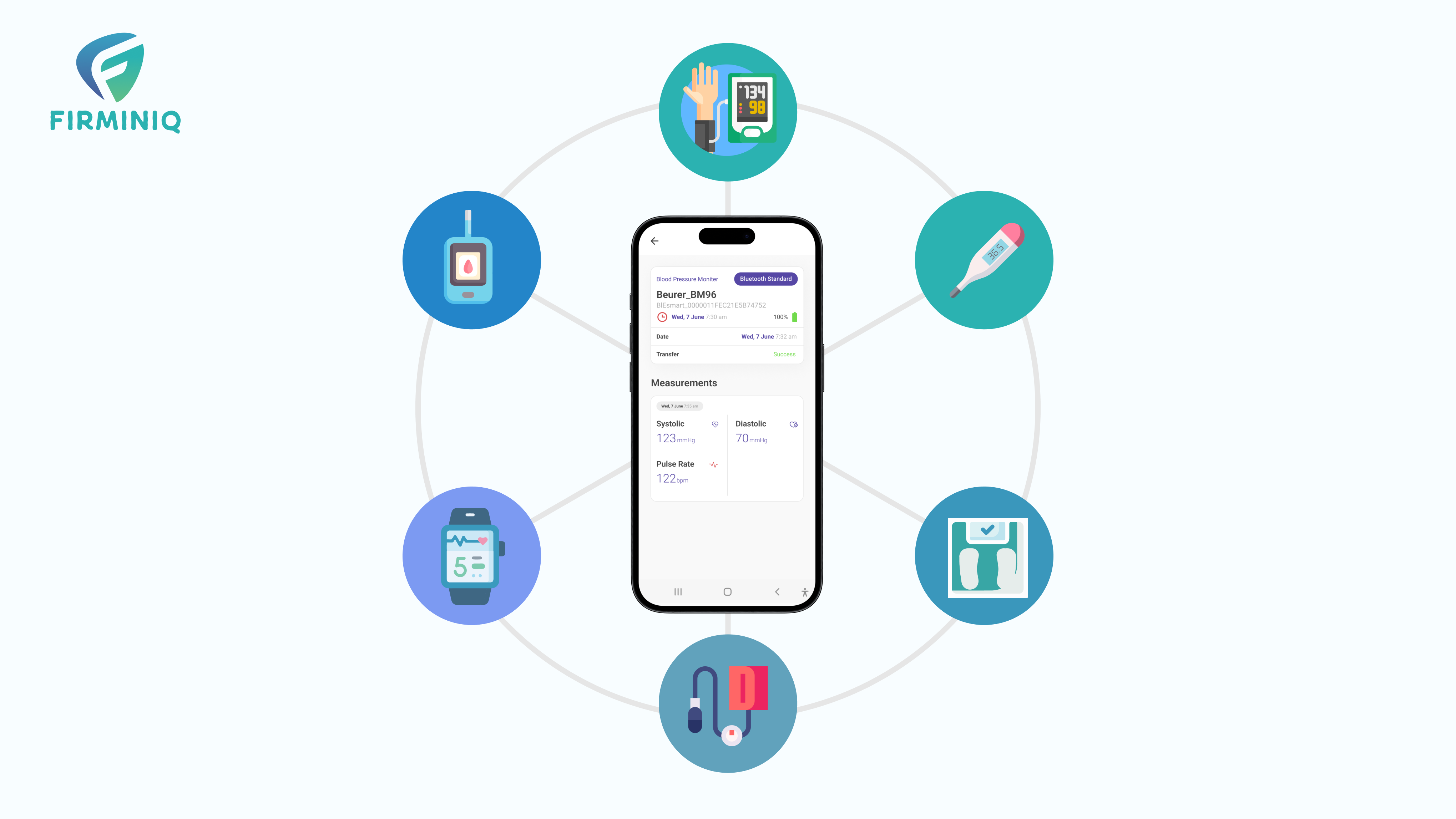
RPM enables providers to monitor patients remotely using wearable devices, mobile apps, and cloud platforms. This is especially valuable for managing chronic conditions like diabetes, hypertension, and heart disease, the conditions that are often prevalent and poorly managed in rural areas.
Key benefits of RPM for providers include:
- Reduced hospital admissions: Timely intervention prevents health deterioration.
- Improved patient engagement: Patients become more active participants in their care.
- Efficient use of limited resources: Fewer in-person visits mean more time for critical cases.
- Data-driven care: Continuous monitoring helps with proactive decision-making.
Step-by-Step Guide to Implementing RPM
1. Assess Community Needs
Start by understanding the health priorities of the population to be served. Identify the most common chronic illnesses, availability of healthcare services, and existing gaps in care delivery. This helps determine the kind of monitoring that will be most impactful — such as glucose monitoring for diabetic patients or blood pressure tracking for hypertensive individuals.
2. Set Clear Goals
Define what you want to achieve with RPM. Your goals could include reducing hospital readmissions, improving medication adherence, or increasing access to regular checkups. Clear goals will help you choose the right technology and measure success effectively.
3. Choose the Right Technology
In low-resource settings, simplicity and affordability are key. When selecting an RPM solution, prioritize those that work well on basic smartphones and can function in low-bandwidth environments. A user-friendly interface is essential, and multi-language support can make adoption much easier in diverse communities. Focus on tools that monitor core vitals like blood pressure, glucose levels, oxygen saturation, and heart rate. Solutions that offer offline functionality and auto-sync when the internet becomes available can be effective. Rather than seeking complex features, concentrate on what’s truly necessary for your patients and care teams.
4. Partner with the Right Vendors
Working with the right vendor is critical to the success of RPM implementation, especially in rural and underserved areas. Seek vendors who understand the challenges of low-resource settings and can provide customizable platforms that align with your workflow. Look for those who offer localized training and support, making it easier to go onboard and troubleshoot in real-time. Cost is a significant factor, so explore vendors with flexible or scalable pricing models, and consider those offering device support. Choose vendors that can support you through setup, training, and ongoing assistance to reduce the burden on your internal teams.
5. Train Healthcare Staff
Your frontline staff—including nurses, community health workers, and clinic support—will be the driving force behind the success of your RPM program. It’s important to educate them on how to onboard patients effectively, interpret the incoming health data, and act on alerts or abnormalities in a timely and appropriate way. Establishing clear escalation protocols will help staff know when and how to involve higher-level clinicians. When healthcare staff are confident and comfortable with both the technology and the workflow, it leads to smoother implementation and better patient outcomes.
6. Educate and Onboard Patients
Patient participation is essential for any RPM initiative to succeed. However, in rural areas, patients may be unfamiliar or skeptical about remote care. Use simple, culturally appropriate language to explain how RPM works and how it can improve their health. Visual guides, printed handouts, and demo videos can help build understanding. If possible, consider sending health workers on home visits to help set up devices and provide initial training. Involving caregivers or family members in the process often improves adherence. The more empowered and comfortable patients feel, the more likely they are to consistently use the technology.
7. Ensure Data Privacy and Compliance
Even in resource-constrained areas, patient data must be treated with the utmost confidentiality. Ensure that the RPM devices you use are secure and offer encryption features. Always obtain patient consent before beginning any form of health monitoring and be sure the data is stored and shared in compliance with local healthcare data protection regulations. Building this layer of trust is essential, both ethically and legally, and reinforces your commitment to responsible care delivery.
8. Monitor and Adjust Workflows
Implementation doesn’t end after deployment. It’s vital to continuously assess how well your RPM program is performing. Are patient vitals being tracked regularly? Are alerts being acknowledged and acted upon swiftly? Are patients dropping off or facing usage issues? Monitoring these aspects helps you identify gaps or bottlenecks in the system. Use feedback to refine your processes, retrain staff where necessary, and optimize the technology to better meet the needs of both providers and patients. Flexibility and continuous improvement are key to long-term success.
Final Thoughts
Implementing RPM in low-resource settings isn’t without its hurdles, but the rewards are far greater. With thoughtful planning, the right partnerships, and a patient-centric approach, RPM can become a powerful tool for equity in healthcare. It bridges the distance between patients and providers, supports better chronic disease management, and makes smart use of limited resources.
For providers committed to creating change in underserved communities, RPM isn’t just possible, it’s transformative. It’s a chance to reimagine care delivery and bring consistency, dignity, and better health outcomes to those who need it most.
Ready to take the first step? Our team can help you build a RPM solution tailored for low-resource settings. Contact us for more information.