In many rural and remote regions, accessing consistent and quality healthcare remains a persistent challenge. Patients often travel long distances to reach clinics, face delays in diagnosis and treatment, and struggle with limited availability of specialists. These barriers not only affect health outcomes but also increase the burden on local healthcare providers who work tirelessly with constrained resources.
Remote Patient Monitoring (RPM) and Telehealth are emerging as efficient solutions to bridge this gap. By bringing care to the patient, regardless of their location, these digital health tools empower providers to monitor chronic conditions, offer timely consultations, and enhance patient engagement. More than just convenience, they represent a new standard of care that is continuous, connected, and truly inclusive.
In this post, we’ll explore the challenges rural areas face, how RPM and Telehealth are revolutionizing rural healthcare delivery, the benefits they bring to both patients and providers, and ways to successfully implement these solutions in underserved regions.
The Rural Healthcare Landscape: Challenges and Disparities
Rural healthcare providers face a unique set of challenges:
- Provider Shortages: Many rural areas suffer from a dearth of healthcare professionals, with some counties lacking even a single primary care physician.
- Geographical Barriers: Patients often have to travel long distances for basic healthcare services, leading to delays in diagnosis and treatment.
- Economic Constraints: Limited funding and resources hinder the ability of rural healthcare facilities to adopt new technologies or expand services.
- Higher Disease Burden: Rural populations often experience higher rates of chronic diseases, mental health issues, and substance abuse, exacerbated by limited access to care.
Telehealth & RPM: Bridging the Gap
In rural communities, where healthcare infrastructure is often limited, digital health solutions like Telehealth and RPM are proving to be game changers. These technologies enable patients to receive timely, high-quality care without the burden of travel or physical visits.
Telehealth uses digital communication tools to connect patients with healthcare providers across distances. This results in:
- Increased Access to Specialists: Patients can consult with specialists remotely, eliminating the need for long and costly journeys.
- Timely Interventions: Early diagnosis and treatment can be initiated promptly, leading to better outcomes.
- Cost Savings: Reduced transportation and related expenses make care more affordable.
A study highlighted that telehealth visits among rural Medicare beneficiaries increased at an annual growth rate of 28% from 2004 to 2013.
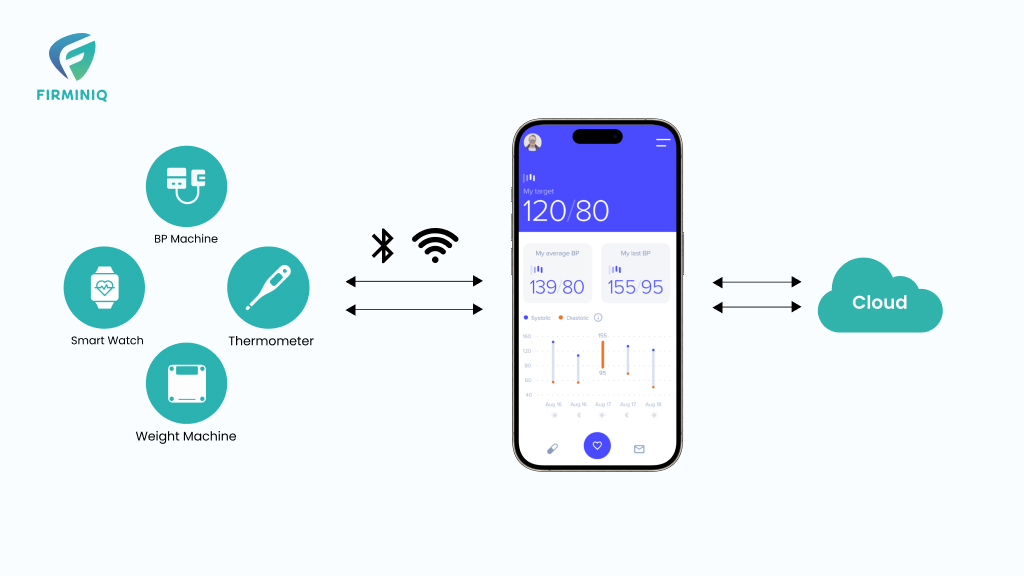
RPM complements telehealth by enabling continuous tracking of a patient’s health through connected devices. Key benefits include:
- Chronic Disease Management: Conditions like diabetes, hypertension, and heart disease can be managed more effectively through regular monitoring.
- Reduced Hospital Readmissions: Providers can detect warning signs early and intervene before complications arise.
- Patient Empowerment: With access to their health data and ongoing support, patients take greater ownership of their wellness journey.
Together, Telehealth and RPM not only extend the reach of care but also redefine what accessible and efficient healthcare looks like for underserved populations.
Overcoming Barriers to Adoption
Despite the evident benefits, several barriers hinder the widespread adoption of telehealth and RPM in rural areas:
- Infrastructure Limitations: Inadequate broadband connectivity hampers the effectiveness of telehealth services.
- Financial Constraints: High initial setup costs and limited reimbursement models deter healthcare providers.
- Digital Literacy: Both patients and providers may lack the necessary skills to effectively use telehealth technologies.
- Regulatory Challenges: Licensing and cross-state practice regulations can complicate the delivery of telehealth services.
According to a National Library of Medicine (NLM) study, rural hospitals in lower-middle socioeconomic status areas were 33.5% less likely to have adopted RPM for chronic care management compared to those in higher SES areas.
The Road Ahead: Strategies for Effective Implementation
To fully harness the potential of telehealth and RPM in rural healthcare, the following strategies are essential:
- Infrastructure Development: Investing in broadband expansion to ensure reliable internet connectivity.
- Financial Incentives: Implementing reimbursement models and grants to support the adoption of telehealth technologies.
- Training and Education: Providing training programs for healthcare providers and patients to enhance digital literacy.
- Policy Reforms: Streamlining licensing processes and establishing clear regulations to facilitate telehealth services across regions.
Embracing a Connected Future
Telehealth and RPM are not mere technological advancements; they represent a paradigm shift in delivering equitable healthcare. For rural communities, these tools are vital in overcoming longstanding barriers, ensuring that quality healthcare is not a privilege of geography but a universal right. By embracing these innovations, rural healthcare providers can build stronger connections, foster healthier communities, and pave the way for a more inclusive healthcare system.
Ready to strengthen rural outreach and deliver smarter care? Let’s connect and explore how we can support your transformation journey.